Not only are we facing shortages in critical antibiotic supplies, but also dealing with increasing antibiotic resistance at the same time. As a race, we’re becoming increasingly fragile. As Americans (well, most readers of this blog are), we have had clean water and food and excellent medical care. The pathogens that regularly assault most people on this planet (and thus test and build up their immune responses) have been far removed from us. We are the most fragile people on the planet. It’s not a good situation to be in.
We have to do everything we can to gain an advantage, especially when it comes to medicine and menacing bacteria. What many people don’t realize is that there are several medicinal herbs that work synergistically with conventional antibiotics. This is especially important as we deal with antibiotic resistance. Using the right herb can also help reduce the time for healing to occur as well as reduce the number of pills that have to be taken, thus extending the supplies. Unfortunately, most physicians are completely unfamiliar with the use of medicinal herbs. Fortunately, you can educate yourself and be prepared when bacteria strike.
The left column of the table below lists some commonly used antibiotics. The center column indicates which herbs can be used to maximize the efficacy of that antibiotic. The right column notes particular conditions or bacteria where the combination of the antibiotic and herb are particularly effective.
|
Antibiotic |
Herbs |
Notes |
|
|
Gram-negative bacteria[3] |
|
|
Ampicillin |
Japanese barberry[4], juniper[5] [6], nasturtium[7], pomegranate[8], thyme[9] |
|
|
Bacitracin |
|
|
|
Ceftriaxone |
Isatis[12] |
MRSA |
|
Chloramphenicol |
|
|
|
Ciprofloxacin |
MRSA (isatis), Klebsiella pneumoniae (rosemary) |
|
|
Clarithromycin |
H. pylori |
|
|
Erythromycin |
|
|
|
Fluconazole |
Japanese barberry[23] |
|
|
Gentamycin |
MRSA (isatis) |
|
|
Oxacillin |
|
|
|
Penicillin |
MRSA, meningitis (piperine) [32] |
|
|
Polymyxin b |
Ginger[33] |
|
|
Streptomycin |
Ginger[34] |
|
|
Tetracycline |
Staphylococcus |
|
|
TMP SMZ |
|
|
|
Tobramycin |
Ginger[40] |
|
This table highlights just a few of the antibiotic-herb synergisms that have been found effective in clinical trials. Herbs have been employed for hundreds to thousands of years to treat infections. Building a good supply of these common herbs will extend your supply of antibiotics and hasten healing. However, keep in mind that these herbs are medicine. They do interact with other drugs and should only be used as advised by licensed medical personnel.
Links to related posts:
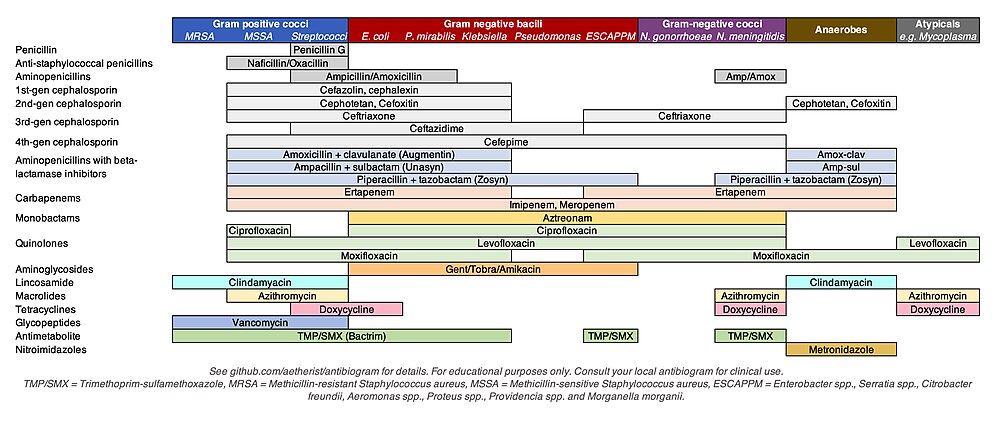
Antibiotic Chart to Guide Acquisition
OK, there are just too many today. Go to the search bar on the right and type in the herb, antibiotic, or medical condition of interest to you.
[1] Stephen Buhner, Herbal Antibiotics, 2012, 238.
[2] Stephen Buhner, Herbal Antivirals, 2013, 219.
[3] Stephen Buhner, Herbal Antibiotics, 2012, 238.
[4] Stephen Harrod Buhner, Herbal Antibiotics, 2012, 166.
[5] Stephen Harrod Buhner, Herbal Antibiotics, 2012, 186.
[6] Rajinder Raina, et al., “Potential of Juniperus communis L. as a Nutraceutical in Human and Veterinary Medicine,” Heliyon, August 2019, Vol 5 No 8, https://www.ncbi.nlm.nih.gov/pmc/articles /PMC6726717/ (accessed 2 February 2021).
[7] Monica Butnariu, et al., Antimicrobial and anti-inflammatory activities of the volatile oil compounds from Tropaeolum majus L. (nasturtium), African Journal of Biotechnology, 29 June 2011, Vol 10 No 31, https://academicjournals.org/article/article1380902607_Butnariu%20and%20Bostan.pdf (accessed 9 December 2021).
[8] Stephen Harrod Buhner, Herbal Antibiotics, 2012, 215.
[9] Stephen Harrod Buhner, Herbal Antibiotics, 2012, 213.
[10] Stephen Harrod Buhner, Herbal Antibiotics, 2012, 235.
[11] Stephen Harrod Buhner, Herbal Antibiotics, 2012, 213.
[12] Z. C. Yang, et al., The synergistic activity of antibiotics combined with eight traditional Chinese medicines against two different strains of Staphylococcus aureus, Colloids Surf. B Biointerfaces, 2005, Vol 41, https://pubmed.ncbi.nlm.nih.gov/15737531/ (accessed 18 September 2021)
[13] Monica Butnariu, et al., Antimicrobial and anti-inflammatory activities of the volatile oil compounds from Tropaeolum majus L. (nasturtium), African Journal of Biotechnology, 29 June 2011, Vol 10 No 31, https://academicjournals.org/article/article1380902607_Butnariu%20and%20Bostan.pdf (accessed 9 December 2021).
[14] Stephen Harrod Buhner, Herbal Antibiotics, 2012, 215.
[15] Z. C. Yang, et al., The synergistic activity of antibiotics combined with eight traditional Chinese medicines against two different strains of Staphylococcus aureus, Colloids Surf. B Biointerfaces, 2005, Vol 41, https://pubmed.ncbi.nlm.nih.gov/15737531/ (accessed 18 September 2021)
[16] Stephen Harrod Buhner, Herbal Antibiotics, 2012, 215.
[17] SF van Vuuren, et al., The antimicrobial activity of four commercial essential oils in combination with conventional antimicrobials, Letters in Applied Microbiology, April 2009, Vol 48 No 4, https://pubmed.ncbi.nlm.nih.gov/19187494/ (accessed 19 January 2022).
[18] Stephen Harrod Buhner, Herbal Antibiotics, 2012, 235.
[19] Stephen Harrod Buhner, Herbal Antibiotics, 2012, 201.
[20] Stephen Harrod Buhner, Herbal Antibiotics, 2012, 186.
[21] Rajinder Raina, et al., “Potential of Juniperus communis L. as a Nutraceutical in Human and Veterinary Medicine,” Heliyon, August 2019, Vol 5 No 8, https://www.ncbi.nlm.nih.gov/pmc/articles /PMC6726717/ (accessed 2 February 2021).
[22] Stephen Harrod Buhner, Herbal Antibiotics, 2012, 213.
[23] Stephen Harrod Buhner, Herbal Antibiotics, 2012, 166.
[24] Stephen Harrod Buhner, Herbal Antibiotics, 2012, 235.
[25] Z. C. Yang, et al., The synergistic activity of antibiotics combined with eight traditional Chinese medicines against two different strains of Staphylococcus aureus, Colloids Surf. B Biointerfaces, 2005, Vol 41, https://pubmed.ncbi.nlm.nih.gov/15737531/ (accessed 18 September 2021)
[26] Stephen Harrod Buhner, Herbal Antibiotics, 2012, 215.
[27] Stephen Harrod Buhner, Herbal Antibiotics, 2012, 166.
[28] Stephen Harrod Buhner, Herbal Antibiotics, 2012, 215.
[29] Z. C. Yang, et al., The synergistic activity of antibiotics combined with eight traditional Chinese medicines against two different strains of Staphylococcus aureus, Colloids Surf. B Biointerfaces, 2005, Vol 41, https://pubmed.ncbi.nlm.nih.gov/15737531/ (accessed 18 September 2021)
[30] Stephen Harrod Buhner, Herbal Antibiotics, 2012, 213.
[31] Stephen Buhner, Herbal Antibiotics, 2012, 245.
[32] Stephen Buhner, Herbal Antibiotics, 2012, 245.
[33] Stephen Harrod Buhner, Herbal Antibiotics, 2012, 235.
[34] Stephen Harrod Buhner, Herbal Antibiotics, 2012, 235.
[35] Stephen Harrod Buhner, Herbal Antibiotics, 2012, 235.
[36] Stephen Harrod Buhner, Herbal Antibiotics, 2012, 215.
[37] Stephen Harrod Buhner, Herbal Antibiotics, 2012, 213.
[38] Florian M Wagenlehner, M et al, Non-Antibiotic Herbal Therapy (BNO 1045) versus Antibiotic Therapy (Fosfomycin Trometamol) for the Treatment of Acute Lower Uncomplicated Urinary Tract Infections in Women: A Double-Blind, Parallel-Group, Randomized, Multicentre, Non-Inferiority Phase III Trial, Urologia internationalis 2018, Vol 101 No 3, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6262678/ (accessed 10 December 2021).
[39] R Stange, et al., Results of a randomized, prospective, double-dummy, double-blind trial to compare efficacy and safety of a herbal combination containing Tropaeoli majoris herba and Armoraciae rusticanae radix with co-trimoxazole in patients with acute and uncomplicated cystitis, Res Rep Urol., 2017, Vol 9, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5359132/ (accessed 10 December 2021).
[40] Stephen Harrod Buhner, Herbal Antibiotics, 2012, 235.
25 january 2022